Volume 21, Issue 1 January/February 2011 | Download PDF

Figure 1. Bony prominences with decubiti (pressure sores)
Fitting a prosthesis is complicated because parts of the human body are used for tasks for which they are not designed. The skin/prosthesis interface is at fault for many complications. Here, a synthetic material, such as silicone or plastic, is in constant contact with the skin. Skin is not well-suited for this type of material contact. Skin problems are one of the most common conditions affecting lower-limb prosthetic users today. Skin problems are experienced by approximately 75 percent of amputees using a lower-limb prosthesis. In fact, amputees experience nearly 65 percent more dermatological complaints than the general population.

Figure 2. Allergic contact dermatitis
Abnormal mechanical and thermal conditions are introduced in a prosthesis, such as socket contact against the skin. This can traumatize tissue by excessive tension, friction or heat. Additionally, the skin reacts to increased temperature with perspiration, which is unable to evaporate because of the closed prosthetic environment. This results in more heat and moisture softening the skin, thereby disrupting normal integrity (maceration).

Figure 3.Irritant contact dermatitis with exco-riation (excessive scratching which breaks thesurface of the skin – circled)
Pressure is another mechanical issue introduced in a prosthetic socket. Certain parts of the human anatomy are well-suited to disperse pressure, such as the fat pad of the heel. With amputation, the normal pressure-distributing anatomy is missing or altered. Therefore your prosthetist must use anatomic areas not well-suited for weight-bearing pressures. Improper socket fit can increase pressure and accelerate skin breakdown. Pressure sores can often be corrected with minor prosthetic adjustments. However, sometimes pressure areas can be more significant and require recovery time out of the prosthesis and/or a complete new socket fit.

Figure 4. Negative pressure hyperemia in an above-knee limb
Irritant contact dermatitis and allergic contact dermatitis are two more common problems effecting prosthetic users. Either of these can occur when the skin is exposed to a material that creates a skin aggravation. If a known irritant or allergic component exists in the patient’s prosthesis, it should be switched to another material. Furthermore, both conditions can be treated with topical steroids or a barrier cream. Several over-the-counter (OTC) topical preparations are available for these conditions, such as hydrocortisone and zinc oxide. Untreated, dermatitis can lead to chronic inflammation, cellular damage and carcinogenesis (cancer). Therefore, we urge all prosthetic users to see a physician when they have failed conservative therapy or have a lesion that won’t heal. It is imperative that these lesions are evaluated so that various forms of cancer can be ruled out.
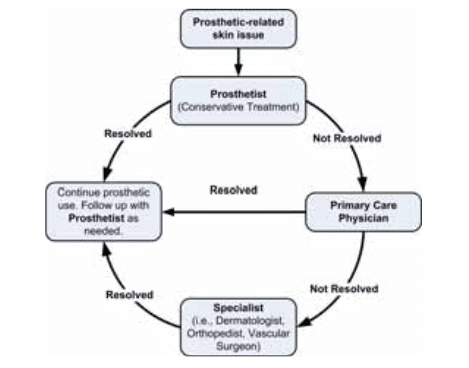 If you encounter a skin problem that you are unable to resolve or that will not heal, then the first step is to see your prosthetist. The prosthetist can then determine if the problem can be resolved prosthetically or through other conservative means. If not, the prosthetist may refer you to your primary care physician or a specialist (see flow diagram).
If you encounter a skin problem that you are unable to resolve or that will not heal, then the first step is to see your prosthetist. The prosthetist can then determine if the problem can be resolved prosthetically or through other conservative means. If not, the prosthetist may refer you to your primary care physician or a specialist (see flow diagram).Skin issues are very common among amputees. Because amputees require an unusually high demand from their skin, and because not wearing a prostheses is often not an option, they sometimes dismiss the importance of hygiene and monitoring of their skin. Skin issues need to be taken seriously. A simple skin breakdown can lead to more severe problems, such as infection, cancer, osteomyelitis (bone infection), and ultimately revision surgery. Start with your prosthetist to determine, and hopefully resolve, the problem. If your prosthetist cannot find a solution, you may need to consult a specialist, such as a dermatologist.


