Volume 15 · Issue 1 · January/February 2005
by Douglas G. Smith, MD

Now, our attention turns to two higher amputation levels – the hip disarticulation and the transpelvic amputation, also known as the hemipelvectomy.
These amputations mean the loss of three joints – the hip, the knee and the ankle. Although there’s no way to predict with certainty who will recover best from an amputation, generally people who have these high-level amputations face much greater challenges. Trying to overcome the loss of three weight-bearing joints, rather than one or two, is extremely complicated. Living with a transfemoral amputation is about 10 times as tough as living with a transtibial amputation, and living with a hip- or pelvic-level amputation is perhaps 100 times harder. Walking, standing, and even sitting balance – something that most of us take for granted – are greatly affected by amputations at the hip or pelvis.
In addition to the physical impact of these hip- and pelvic-level amputations, they also have an increased impact on self-image. There’s increased worry and stress as these surgeries start encroaching on that personal area involved in central body functions and gender identity. Sometimes, the surgery affects bowel, bladder or sexual functions. Most of the time, it does not. But either way, it starts involving the core of the body. No longer does amputation focus solely on the loss of some or all of a limb. The emotional and psychosocial aspects of these amputation levels can be even greater than those for other amputations.
I’m a big believer in support groups, but, unfortunately, some people with hip- or pelvic-level amputations may feel left out and even isolated during meetings. There are fewer people with these high-level amputations, and often the focus of support groups can be on the issues and challenges faced by the majority. The perspective is different. Many of my patients who’ve had amputations at the hip or pelvis tell me that, while they enjoy some aspects of a support group, they often don’t feel totally included or in sync with the other members. They say some of the issues brought up during meetings may not be relevant to them, and their own issues may not be relevant to the others. If the group has a large number of transtibial or transfemoral amputees, the discussions may focus mainly on the issues they face. A person with an amputation below the hip and pelvis may not be dealing with body core function and image issues so he or she likely wouldn’t have anything to say about these issues or even know what to ask. It may be difficult for other members of the group to understand or connect emotionally with the concerns of a person with a hip- or pelvic-level amputation. Likewise, a person with one of these high amputation levels may be reluctant to bring up some issues with those who aren’t in a similar situation.
“Could a greater miracle take place than for us to look through each other’s eyes for an instant?” – Henry David Thoreau/ essayist, poet, philosopher
 The Hip Disarticulation
The Hip Disarticulation
Hip disarticulation is the surgical removal of the entire lower limb at the hip level. A traditional hip disarticulation is done by separating the ball from the socket of the hip joint, while a modified version retains a small portion of the proximal (upper) femur to improve the contours of the hip disarticulation for sitting. A hip disarticulation results most often from trauma, tumors and severe infections, such as necrotizing fasciitis (commonly referred to as flesh-eating bacteria). Less often, it results from vascular disease and complications of diabetes.
In past decades, hip disarticulation was the common treatment for cases of aggressive cancer in the lower limbs. The surgeon’s goal was to surgically remove all of the tumor cells and minimize any chance that the cancer would recur so the amputation was done all the way up in the hip area. Today’s treatment can include surgery, chemotherapy or radiation modalities to destroy tumor cells. Because of these additional modalities, we can now perform different types of surgery, and the amputation site can be lower. We can also do more limb salvages now. Many patients, especially children, are candidates for surgical resections and replacement of missing skeleton with donor bone or metal implants. Unfortunately, salvage is not always possible, and amputation is still an occasional treatment for both childhood and adult cancers of the lower limb.
The Transpelvic Amputation
Transpelvic amputation is the removal of the entire lower limb, plus a portion of the pelvic bones. It occurs in a skeletal zone that can include, from the socket on the outside to the spinal column in the middle, the acetabulum, ischium, rami, ilium and sacrum. Transpelvic amputations result mostly from very severe trauma, tumors, and, specifically for spinal-cord-injury patients, recurring severe ulcerations and infections.
One extremely important aspect of problems at the transpelvic level is the higher risk of mortality. It’s a sad truth that many people don’t survive the disease or injury that can lead to amputation at this level. And amputations at this level carry a significant death rate at the time of surgery or during hospitalization immediately thereafter. Some studies show that up to one-third of the people hospitalized for transpelvic surgery don’t survive. Occasionally, these injuries result from a crushing injury, such as a cave-in at a construction site, or an explosion. More frequently, the injury results from a high-speed impact with a post on a motorcycle, all-terrain vehicle or snowmobile that causes shearing trauma up through the pelvis. With injuries like these, the person has a more acute risk to life.
As previously noted, the transpelvic amputation removes more than a limb. By removing part of the pelvic bones, and possibly the organs involved in reproduction, bowel and bladder functions, we’re starting to lose parts of the core center of the body. These amputations, therefore, have profound effects that extend beyond the loss of a limb and walking function. They can seriously impact sitting, with difficulties in balance, support and weight distribution, which can lead to a higher risk for pressure ulcerations and sores. In addition, these amputations can impact bowel, bladder and sexual functions and the symmetrical nature of the lower core center of the body.
Surgery
Hip disarticulation and transpelvic amputation surgeries frequently require more variability at the amputation site than do other amputations of the lower limb. Ingenuity and creativity may be demanded of the surgeon because the amount of tissue lost to injury, disease or infection is different in every case. Also, there’s not as much soft tissue to work with for wound closure and padding at these hip-level amputation sites as we find in the calf or thigh areas. When injury, disease or infection requires amputation farther down the leg, the person and the surgeon usually agree it is best to do the amputation at a level above the problem area. For example, if there are severe problems in the foot or ankle area that lead to amputation, the amputation is usually performed up in the calf, above the problem area. This moves the amputation outside the zone of injury, disease or infection and usually provides fairly normal tissue for padding. Moving up the limb also better promotes healing and comfort. Similarly, if there are problems around the knee area, the amputation site is typically moved up to the thigh, again above the area of injury, disease or infection.
But there’s simply no room to move higher when the injury, disease or infection involves the hip or pelvic area. This is the first amputation level in the lower limb where there isn’t an option to keep moving up. It’s a physical reality; there’s nowhere higher to go, and the surgical team must do the best it can under the circumstances. That means greater challenges during surgery. Surgeons need to be more creative because they’re working directly in the problem zone. And because they can’t move the amputation site to an area where there’s normal tissue for padding and closure, the closures become more fragile.
This lack of extra soft tissue can lead to scarring and a need for special flaps for skin grafts. Age can also play a factor. Scarring and grafts tend not to be as big a problem for children as they are for older adults. Many younger children amaze their physicians and therapists because they master walking and sitting, learning to live with the tremendous losses that amputations around the hip bring. While adults also must overcome these losses, it’s far more difficult for them to find similar success with prostheses. Adults have to work a heck of a lot harder at it! We’ll examine this concept in more detail in Part 2 of this series.
The surgical team tries to shape the bone surfaces so that they can take weight while sitting and standing and to use as much padding as possible to cover the skeletal surfaces. Depending on availability, the buttock or thigh muscles are typically used for this. The standard procedure is to use the buttock muscles for padding over the hip area. But if these muscles are lost, the next choice would be the quadriceps muscle in the front of the thigh. Sometimes, both the buttock and thigh muscles are lost – and this is a really big problem. Without healthy muscle to provide padding, closure or coverage often depends on secondary healing – essentially allowing Mother Nature to fill in the wound over time – and eventually placing fragile skin grafts. All of this makes the area much more tender and prone to injury, infection or both. Unfortunately, in some of these cases, there simply are no good options.
The basic forms of amputation in the hip area are the modified hip disarticulation, the traditional hip disarticulation and the varying degrees of transpelvic amputation. In a modi- fied hip disarticulation, the entire leg is removed except for the very top part of the femur (thigh bone) around the greater and lesser trochanters (two bump-shaped prominences of bone where the tendons attach below the neck of the femur) and the hip joint’s ball and socket. This provides a smoother surface for the muscles to rest over and can sometimes improve sitting support.
In a traditional hip disarticulation, the top part of the femur is removed, and the hip’s ball and socket are taken apart. The entire femur, including the ball, is removed, while the hip socket is retained.
If the injury or disease involves the socket or pelvic area, a transpelvic amputation may be necessary. The hip socket and parts of the pelvic bones (acetabulum, ischium, rami, and ilium) are removed. There are many variations in how much of the pelvis is removed, depending on the trauma, infection or tumor. Sometimes, even the sacrum (a triangular bone, which is made up of five fused vertebrae just above the coccyx, that forms the base of the spine) may be removed, but we try to avoid this, if possible. When the sacrum is involved in the amputation, it means sacrificing nerves related in varying degrees to bowel, bladder or sexual functions, or some combination thereof.
 A Common Misconception
A Common Misconception
Many people mistakenly assume that the difference between a hip disarticulation and a transpelvic amputation is comparable to the distinction between a knee disarticulation and a transfemoral (above-knee) amputation. They think that by moving up to the next higher amputation level there will be abundantly more soft tissue for wound closure and padding. But the hip disarticulation and transpelvic levels are extremely close to each other skeletally, and both rely on the same muscles for closure and padding. Any problems with insufficient soft tissues won’t change dramatically by moving to a higher level because a transpelvic amputation generally occurs just two inches above a hip disarticulation. The soft tissue envelope doesn’t really change much in those two inches. This misconception is widespread. I’ve had medical professionals ask me, “This hip disarticulation won’t close. Can’t we just do a transpelvic amputation so we can get it closed?” And I have to say, “While the transpelvic amputation will remove more bone, it doesn’t necessarily create more soft tissue or let the soft tissue close with much more ease. The amount of soft tissue for closure changes very little.”
The Possible Impact on Bowel, Bladder and Sexual Functions
I’m often asked whether these amputation levels will have any effect on bowel, bladder or sexual functions. The answer is, “Occasionally.” Typically, a modified hip disarticulation or a true hip disarticulation will have absolutely no effect on these functions, but in special circumstances they might. When there are wounds near the rectal area from the trauma, infection or tumor, a temporary colostomy (an artificial anal opening in the body from the colon) is done for hygienic reasons. The colostomy helps keep the wounds cleaner during the time of wound care and healing. The goal after wound healing commonly is to remove the colostomy and restore normal bowel function. This usually proceeds as planned, but in rare instances, the need for a colostomy becomes permanent.
In a hip disarticulation, the organs for urinary, bowel and sexual functions usually retain function. But there sometimes is a perception of change in that area of the body. That’s because the bowel, bladder and sexual organs are so close to the incisions and surgery sites that they are perceived to be involved. When I’m talking to people before surgery, I tell them that while we are not going to operate on the sexual organs or rectum, the surgery may still have an impact on those areas. Typically, there’s surgical swelling after the amputation, and it may feel as if those personal parts are being pushed to the nonamputated side. As the swelling goes down and the scars heal and contract, it may feel as if the scar tissue now is pulling things back over to the amputated side. This back-andforth phenomenon can be emotionally disturbing. We think of that area of our body as symmetrical. When surgery results in “a shifting of the landscape,” we’re very concerned, even if function is not affected.
The chance of alteration in bowel, bladder or sexual functions increases in a transpelvic amputation, which involves the loss of part of the pelvic bone. Nerve roots in the sacrum at the bottom of the spinal column may be divided. It’s these sacral nerve roots that provide feeling for the bowel and bladder areas. A colostomy for bowel function or urostomy for bladder function may be needed in some cases. While the rectal area and sexual organs are saved in other cases, they may be repositioned. This concept of repositioning can be difficult to visualize.
Repositioning occurs as surgical closure rotates soft tissues, such as when soft tissue from the front of the thigh is pulled back and around to cover the amputation site. The organs aren’t literally moved surgically from one point to another; rather, they are gently pulled, pushed, rotated or twisted as soft tissue is repositioned so that they are no longer symmetrical in the middle.
Certainly, not everybody who undergoes an amputation at the hip or pelvis must contend with changes in any of these functions. Unfortunately, some people are impacted, more often those who undergo a transpelvic amputation rather than those who have a hip disarticulation. There’s no single answer for everybody; it depends on the zone of injury or disease.
The loss of any or all of these functions can be even more emotionally devastating than the loss of one or both legs. And it makes for challenges in the prosthetic fitting. At these amputation levels, the prosthesis incorporates the pelvis; in some cases, it may extend all the way up to the ribs. We don’t want the prosthesis to push against an ostomy (artificial opening) site, however, and it becomes a real challenge, prosthetically, to work around these sites.
Rehabilitation and prosthetic considerations for hip- and pelvic-level amputations are very complex. In the upcoming parts of this series, we will discuss the importance of youth and aging in recovery from these amputations and offer further insights into emotional and personal issues. From the prosthetic point of view, we’ll talk about sockets that incorporate the pelvis and lower body and the technical issues of locating the hip joint. As we’ll see, the goals of recovery are not always as straightforward as they can be for lower-level amputations.
These high amputation levels truly are closer to our core and soul, often bringing us even closer to our own mortality. We are confronted with major changes and must reach deep within ourselves to find new ways to adapt. The course is not always clear, and it is never the same for every person. We don’t always know where the winds of fortune will take us, but each of us must find a way to adjust to them. It’s been said, “We cannot direct the wind, but we can adjust our sails.”



 The Hip Disarticulation
The Hip Disarticulation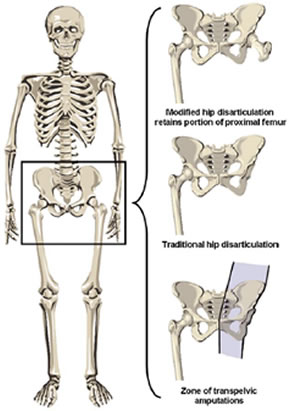 A Common Misconception
A Common Misconception