Volume 14 · Issue 3 · May/June 2004 | Download PDF
by Douglas G. Smith, MD, Amputee Coalition Medical Director
Surgery and Postoperative Care
Part 1 of this series of articles on the transfemoral (above-knee, or AK) amputation level examined various aspects of energy use while walking and some of the many challenges of adjusting to life with this type of amputation. This article will focus on surgery and postoperative management.
Surgery
The transfemoral amputation level teaches surgeons the great importance of muscle reconstruction. A person with a transfemoral amputation can support very little, if any, weight directly on the end of the limb. In addition, the thigh muscles are out of balance after the femur is transected (cut). Therefore, during surgery, two of our goals are to try to regain muscle balance and to better position the femur so that it can take some weight on the side of the thigh.
The term for the surgical technique to reattach muscles to bone following amputation is “myodesis.” There are two main methods for performing this surgery:
- The surgeon can drill holes through the bone and suture (attach) the muscle directly to the bone.
- The surgeon can secure the muscle over the bone and suture it to the periosteum (the thick tissue covering the bone).
There are four major muscle movements in the thigh:
- Forward, which is called flexion
- Back, which is called extension
- In toward the middle, which is called adduction
- Out to the side, which is called abduction.
The abductors and flexors are attached up near the hip. They are above the surgical division in a transfemoral amputation so they usually are not affected by the transection. However, the adductor and extensor muscles are divided because they are attached at the lower end of the thigh. Therefore, in this type of amputation surgery, you lose those muscle attachments that allow you to move your leg inward, such as when you cross one thigh over the other, and to bring your leg back behind you.
Without the adductor and extensor muscles and without myodesis, there’s a natural tendency for the leg to simultaneously go forward into flexion and out to the side in abduction. The surgeon, therefore, needs to reattach muscles to the femoral bone or its periosteum as a counterbalance to the forces of flexion and abduction. Myodesis makes the residual limb stronger, more balanced, and keeps the femur centered in the muscle mass.
You might be asking, “What about the big muscle in the front of the thigh?” That’s called the quadriceps, and it is actually primarily a knee muscle. It plays a small part in hip movement, but chiefly is involved in knee movement.
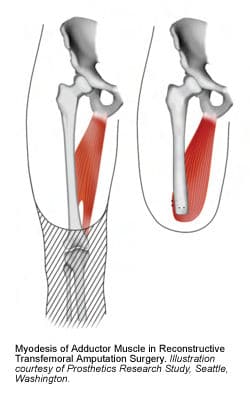
Myodesis may also be beneficial in reducing a collection of tissue called “the adductor roll,” which can form high on the inner thigh above the socket line and can be quite bothersome for some people. Many believe that the adductor roll is caused, in part, by the retraction of muscles that are no longer held in place. The tissue spills out over the top of the socket, and before long a significant roll of soft tissue has accumulated in that area. The socket may dig painfully into this extra tissue. Myodesis helps secure that tissue and seems to reduce the adductor roll for some individuals.
Now that we understand the goals of myodesis, here’s the downside: Muscle doesn’t hold sutures very well, and the transfemoral amputation occurs in an area of muscle that isn’t ideal for holding surgical attachments. Many people don’t realize just how difficult it is to sew into muscle. You may look at a solidly built person, say a bodybuilder, and think, “That’s a lot of strong material to work with.” But appearances from the outside are deceiving. Think of the tissues of the muscles like a mop. The strings of the mop are encased in a plastic wrapper when you buy it. That plastic wrapper is like the fascia, which is the tissue that covers the muscle. Suturing muscle is like sewing through the plastic bag and the strings of the mop. Fascia, like the plastic wrapper, provides some reinforcement, but the individual strands of muscle don’t hold sutures well. And like the strings of a mop, there’s not much between the muscle strands to use as reinforcement. When a suture is inserted in mid-thigh, it drifts downward in the muscle tissue because it can’t be securely attached to anything. If the surgeon tries to go across the strands and loop them together, blood flow is cut off to the end of the muscle.
The fascia is the best available tissue for holding sutures in a transfemoral amputation, but it’s not especially thick around most of the muscles in mid-thigh. In fact, it’s quite thin and can tear easily. Tendon and skin hold sutures well, muscle does not, and fascia at mid-thigh is just so-so. So while myodesis is important, it can be difficult to do securely at this level. In the postoperative period, occasionally there are patients who feel the myodesis stretching out or even pulling free. “Doc, I think I felt something give” is the way they usually describe it.
Transfemoral Amputation and Children
The growth plate located at the bottom of the femur is lost in a transfemoral amputation. This plate provides for 60 to 70 percent of thigh growth. In children, that means the residual limb won’t grow equally with the upper part of the other limb, which becomes increasingly important as the person grows up and enters adulthood. By then, the differences between the two thighs can be significant. What appeared to be a very long transfemoral amputation in a young child turns out to be a very short transfemoral amputation level that’s difficult to fit with a prosthesis when the youngster becomes an adult.
When dealing with osteosarcoma (a type of cancer) in children, one challenge concerns the difficult decision between amputation and limb salvage. Most cases of this cancer happen in children between the ages of 8 and 15, and the disease frequently occurs in the knee area. A knee disarticulation often is not possible, however, because part of the tumor may be located at or near the far (distal) end of the femur. So, by necessity, an amputation must be at the transfemoral level, even though it means the growth plate near the knee will be lost and the residual limb will become shorter as the person grows.
Growth issues can also be a major concern with limb salvage. More often than not, salvage involves removing the end of the femur and replacing it with bone or metal, which does not grow. For young children, salvage can mean a number of surgeries over several years, each designed to add a bit of length to the limb because it’s no longer growing at its proper pace.
When facing the difficult choice between limb salvage or amputation, issues concerning rehabilitation and quality of life afterward must be examined closely before proceeding. We hear exciting news about limbs that are salvaged or even reattached. The typical person often believes this means, “It will be normal again.” Unfortunately, this usually is not the case. These salvaged limbs still have severe limitations. The procedures are complex and frequently there are complications. Even after the person has gone through extensive surgery and rehabilitation, it can be daunting to manage all of the issues of living with a fragile limb – one that is often without normal sensation. Limb salvage, like amputation, can still mean real restrictions, with issues such as functional limitations, durability and pain.
Postoperative Management
In general, for those who have had lower-limb amputations, healthcare professionals have tried to encourage aggressive and active rehabilitation in tandem with wound healing. My mentor, Dr. Ernest Burgess, used to say: “There is no excuse for delay or procrastination waiting for amputations to mature. Maturation will take place concurrent with active return of function.” In other words, “push ahead with the rehab.” Dr. Burgess urged others to overcome the misconception that rehabilitation should come only after the wound heals. He spent much of his professional career designing protocols to safely move forward with rehabilitation while the amputation is still healing. Many of the immediate postoperative casting protocols for partial foot amputations, transtibial amputations and knee disarticulations do include early weight-bearing by allowing some limited walking. Protocols for very aggressive rehabilitation after transfemoral amputations certainly have been offered; unfortunately, these are less successful than those for lower levels. Many rehabilitation programs that use aggressive casting protocols for transtibial amputations have drifted away from them for individuals with transfemoral amputations, primarily because of patient comfort. The end of the femur just cannot support the body’s weight so any immediate postoperative prosthetic device must include the pelvic area.
When amputations are performed at or below the knee, the cast comes up no higher than near the top of the thigh. For a casting protocol to work after a transfemoral amputation, it must come all the way up to incorporate part of the pelvis. Traditionally, casting rings, called brims, are used to help mold the cast in the region at the top of the thigh and buttock. The cast is then extended up around the hip and waist in a spica fashion. Spica means a cast that incorporates the waist. A hip spica is an extremity cast that incorporates the torso. While the top part is a little softer than the full rigid cast, it still comes high up into the groin and around the waist. These casts are designed to keep weight off of the surgical incision and to spread the weight higher up the residual limb. They’re also designed to stay on as the limb volume changes in the postoperative period.
When I first moved my surgical practice to Seattle, I worked with Mr. Joe Zettl, the prosthetist who teamed with Dr. Burgess to pioneer many of these casting techniques. We found that these protocols work well for the hour or two a day when the patient is upright during therapy, but that they are very uncomfortable when the person is lying in bed or sitting in a chair. For the transfemoral amputee, these immediate postoperative prosthesis (IPOP) casts are not designed to be removable. There are hygiene factors to take into account because the cast incorporates the waist and groin. We found that while patients appreciated having this system for the short time they were upright in therapy, they were miserable with it the other 22 hours of the day. Some literally begged us to remove it.
What’s the solution? We found simple techniques that wrap both the amputation site and waist with soft bandages to be effective. In the operating room, plaster splints are initially incorporated in the bandage over the amputation site as a rigid dressing to protect against bumps and bangs. Softer wrapping material comes up over the hip and around the waist. The hip can move more freely, and this also allows for exercises, leg lifts and stretching. It’s not rigid enough to support a foot attachment and allow the person to put weight on it, but it’s much more comfortable. This bandage typically is changed sometime between three and five days after surgery. The person is then fit with a shrinker sock that includes a waist belt. The shrinker sock is an elastic garment measured specifically to fit the length and shape of the amputated limb and to apply gentle compression more at the end of the limb than at the top of the limb. To further control swelling and decrease pain, the person learns massage and towel-pulling exercises. In towel pulling, a towel is draped over the end of the amputation site, and the person holds the ends with each hand and pulls the towel against the end of the amputated limb. This pumps out some of the edema to reduce swelling, and many people say it also lessens pain. They tell me, “It’s a good hurt. It’s sore when I’m doing the towel pull, but it feels so much better when I’m done.”
Another major focus of our immediate postoperative care is to prevent contractures, which are the loss of range of motion at one or more joints. Specifically with a transfemoral amputation, people have trouble with hip contractures from the shortening and wasting away of muscle fibers. For some transfemoral amputees, the hip becomes locked forward in a flexed position. This can make it difficult, sometimes even impossible, to fit the leg with a prosthesis. A helpful exercise to prevent contractures is to stretch the hip backward into extension. The best way to stretch the hip is to lie on your stomach for five to 10 minutes, staying flat at first and later using your hands and arms to push your shoulders, chest and torso up so that your back is arched. Those of you who practice yoga will recognize this as “The Cobra” position. This sounds simple enough, but it’s not that easy for some people, especially those who’ve developed “a little extra” in the belly. Some people haven’t lain on their stomachs in years, and this exercise can be a real challenge for them. At times like this, they don’t think of their therapist as “Mr. Wonderful” or “Ms. Fabulous,” to put it mildly. It’s tough. But hip flexibility really counts so we focus on stretching and encourage folks to do this two or three times every day.
A Note From the Doctor
I had intended this series on transfemoral amputations to be presented in three parts. But as this project has moved forward, it has become increasingly apparent that there are so many aspects to this amputation level – both during surgery and afterward – that it would be a disservice to limit the scope of this discussion in any way. Therefore, it has been expanded to four parts to include discussion of other important issues. The next article will discuss the sometimes-difficult choice of when, or even if, to use a transfemoral prosthesis and other personal, family and ethical concerns. The final article on the transfemoral level will look in-depth at various socket designs, suspension systems and the wide range of new and older prosthetic components.
“Technology presumes there is just one right way to do things and there never is.” – Robert M. Pirsig, author
Next: Mastering the Vital Skills & “When Can Grandpa Get His Leg?”